Tyler Ford
05/25/2021
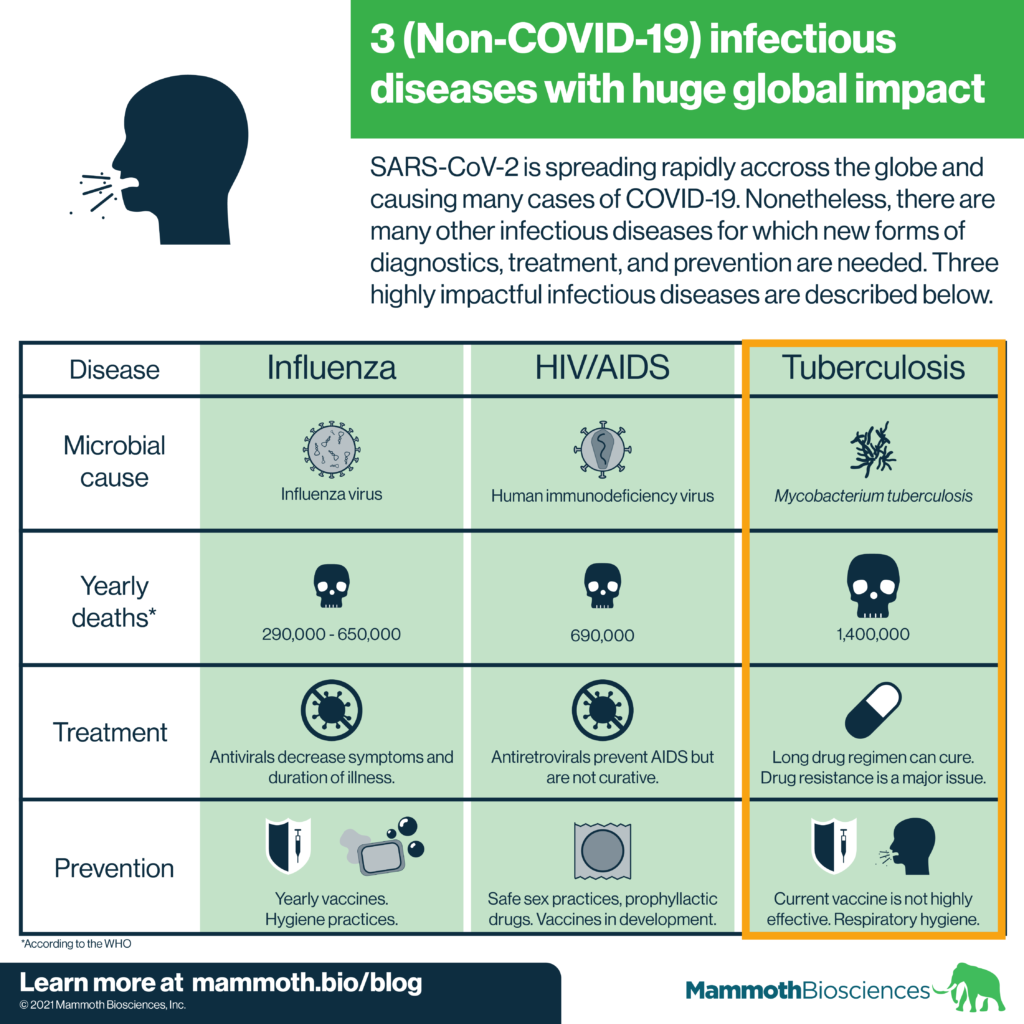
The COVID-19 pandemic rages on, but it’s important to remember that other infectious diseases continue to have huge global impacts. Indeed, COVID-19 may be making it more difficult to address other diseases (Eg. HIV/AIDs, other STIs, antibiotic resistant infections). In this “Infectious Disease Spotlight” series, we cover 3 of the most globally impactful infectious diseases. Just as they are essential in our efforts to stop the spread of COVID-19, new diagnostics will help pave the way to controlling these diseases.
In this post, we cover tuberculosis. Check out our other posts on HIV/AIDS, the flu, Candida auris, and Neisseria gonorrhoeae.
Tuberculosis – a global killer
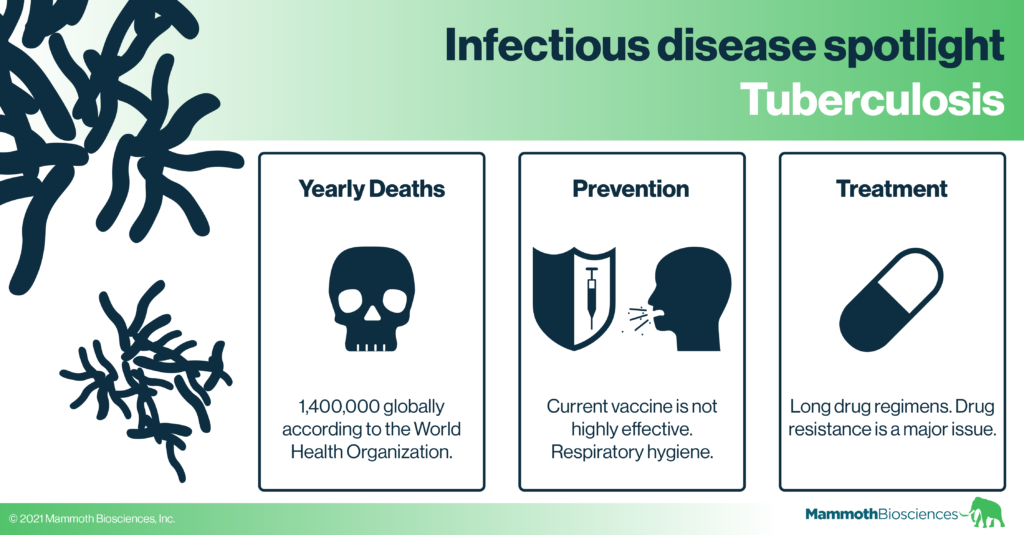
Tuberculosis (TB) is usually a pulmonary disease that can manifest in a variety of ways. It is caused by Mycobacterium tuberculosis infection (WHO Global Tuberculosis Report 2020). The WHO estimates that 1 in 4 people are infected with TB worldwide. In addition, active TB disease killed roughly 1.4 million people globally in 2019 (WHO Tuberculosis fact sheet).
Researchers broadly distinguish between two types of tuberculosis infection:
- Latent TB infection – Individuals with latent TB infection have TB bacteria in their bodies, but do not present symptoms. They will test positive with some but not all types of TB diagnostics. They cannot transmit the virus (Pai et al 2016).
- Active TB disease – Individuals with active TB disease experience a variety of symptoms. These include lung distress, coughing, coughing up blood, fatigue, fever, wasting (becoming weak and emaciated), and death (Pai et al 2016). Those with active TB disease are contagious and can spread TB bacteria through the air (CDC Questions and Answers about TB).
Preventing tuberculosis transmission
Testing, behavioral practices, treatment, and vaccines are the primary ways to prevent tuberculosis transmission.
Once someone with active TB infection is identified, they can be isolated to prevent further transmission. It’s recommended that those who come in close contact with individuals who have active TB disease get tested so they can take the appropriate isolation and/or treatment measures.
Healthcare workers treat active TB disease with a long course of drugs (more on this below). Treatment often eventually clears the infection and will stop future transmission.
It’s important to take special care to prevent TB transmission and treat TB infection in HIV positive individuals. Due to their lowered T cell counts, HIV positive individuals are at greater risk of falling ill or dying of TB infection. The WHO recommends actively testing HIV positive individuals for TB infection and vice versa. With testing, the appropriate treatment measures can be taken as soon as possible.
In terms of vaccines, the only vaccine currently used to prevent severe TB disease is the neonatal Bacille Calmette-Guérin (BCG) vaccine. The BCG vaccine contains a weakened version of a bacterium that causes TB in cows (Vaccine Knowledge Project). It is effective at preventing severe TB disease in children under 5. It loses effectiveness as recipients move into adolescence (Pai et al 2016).
The WHO has prioritized the development of an effective TB vaccine for adults. Thus far at least one TB vaccine has shown promising results. Researchers recently tested this new vaccine in a Phase IIb clinical trial (Tait et al 2019). They found that the vaccine is 50% effective at preventing latently infected HIV- individuals from progressing to active TB disease. This represents great progress, but we need more research to determine if the vaccine affects initial TB infection. More research can also determine if this vaccine is effective in HIV positive individuals.
Tuberculosis diagnostics
There are a variety of ways to diagnose TB infection. These include:
- Skin tests that check for reactions to components of TB bacteria when injected into the skin
- Blood tests that check for immune cell reactions to components of TB bacteria introduced to a blood sample
- Chest X-rays searching for signs of lung abnormalities
- Rapid molecular tests that search for components (DNA and protein) of the TB bacterium in patient samples like spit
- Bacterial culture from patient samples
The WHO recommends increased use of rapid molecular tests for TB diagnosis. These technologies are more specific and sensitive than other diagnostics tools. They can also identify antibiotic resistant TB infections. This is critical because half a million people get drug resistant TB each year. Overall, rapid molecular tests enable quick and effective action against TB infection.
Unfortunately, many regions with high TB prevalence cannot afford or do not have access to the speciality equipment and labs required for molecular tests. Thus, the WHO is pushing for the development of point of care diagnostic tests that healthcare workers can use where TB patients get their medical care. Some such tests already exist. For example, the “Lateral flow urine lipoarabinomannan assay” detects a TB protein in urine. Some of the current point of care tests are considered insensitive but we’ll hopefully see improvement in this area soon!
Critically, the COVID-19 pandemic has decreased TB testing, reporting, and treatment. This may be due to standard TB testing centers diverting resources to the pandemic. The changes in TB surveillance and treatment wrought by the pandemic highlight the need to develop diagnostic tests (like CRISPR diagnostics) that are available when and where patients need them. Ideally these tests will use different supply chains than standard testing procedures such as PCR.
Finally, the WHO actively promotes the development of new diagnostic technologies that can find individuals who are high risk for developing active TB disease. Such diagnostics would make it possible to prioritize treatments and resources to those who are most at risk of dying from TB.
Treatment
Both latent TB infection and active TB disease can be treated with long courses (sometimes >6 months) of drugs. However, new drugs and treatments are needed for two key reasons:
- Patients may find it difficult to adhere to the long (and sometimes complex) drug regimens required for effective TB treatment.
- Many people have drug-resistant TB infections. These can’t be treated with standard TB drugs, require even longer courses of treatment, and have increased toxicity.
In addition, failure to adhere to treatment regimens can lead to the evolution of increased drug resistance. Thus we need new treatments to shorten the duration of treatment and make it possible to fight resistant infections.
Researchers are developing and testing a variety of new TB treatments. You can learn more about these in the TB research and innovation section of the WHO’s Global Tuberculosis Report.
Conclusion
The last decade has seen decreases in deaths and cases of TB across many regions. However, TB is under-researched and under-funded. The pandemic has shown us that we must better prepared to tackle diseases like TB as new infectious diseases arise. This will involve investing more time and money in infectious disease diagnostics, treatment, and prevention. If we develop effective infectious disease infrastructure, we can save many lives!