Tyler Ford
09/07/2021
Antibiotics have been an essential tool of modern medicine since the 1940s. They’ve cured countless bacterial infections and saved many lives. Unfortunately, many bacteria are evolving resistance to antibiotics. In addition, other microbes like fungi, viruses, and parasites are also evolving resistance to the drugs used to treat them. Researchers call this cumulative problem “antimicrobial resistance.” This growing threat results in more than 1,000,000 deaths per year globally. That number is expected to increase as the impacts of this “silent pandemic” become ever more prevalent.
This series aims to provide a finer point on the impacts of antimicrobial resistance. It highlights some of the antimicrobial resistant pathogens that the US Centers for Disease Control (CDC) considers “Urgent Threats.” These include:
- Neisseria gonorrhoeae
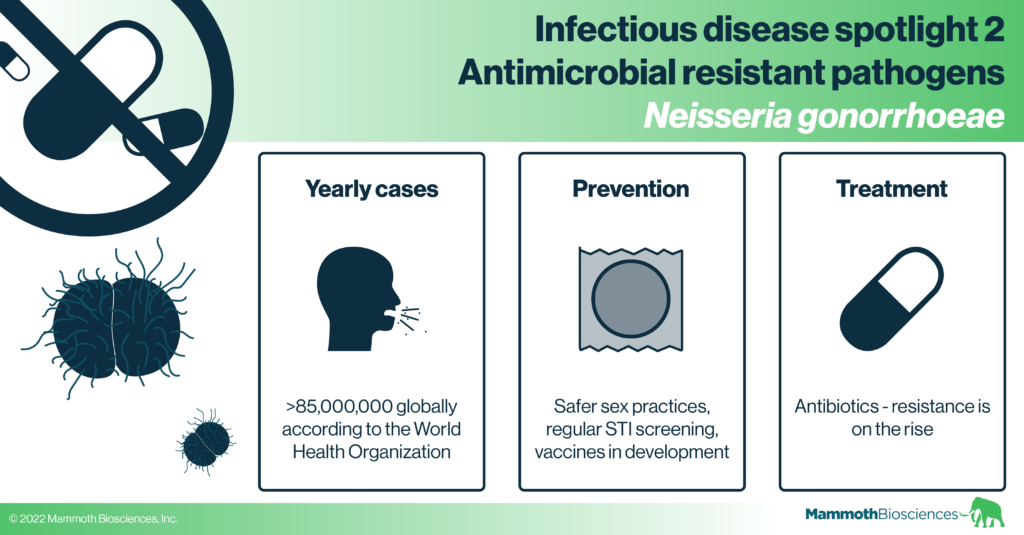
Today we start with Neisseria gonorrhoeae. This pathogen causes the common sexually transmitted infection (STI) gonorrhea.
Check out our previous “Infectious disease spotlight” series for posts on the flu, HIV/AIDS, and tuberculosis.
Check out our other posts on HIV/AIDS, the flu, tuberculosis, and Candida auris.
Neisseria gonorrhoeae general biology and transmission
Neisseria gonorrhoeae is very similar to certain “commensal bacteria.” That is, bacteria that are a normal part of the human microbiome. Indeed, it’s believed that Neisseria gonorrhoeae evolved from commensal bacteria (Seifert 2019).
This pathogen usually infects tissues of the urogenital, rectal, and oropharyngeal mucosal surfaces. Thus, it is usually transmitted through various types of sexual intercourse.
It is possible to culture Neisseria gonorrhoeae samples in vitro. However, most model systems fail to recapitulate this pathogen’s complex natural lifestyle. This is because there are many interactions between the bacteria, mucosal cells, and the immune system. These all impact the life and transmissibility of the pathogen.
Unfortunately, Neisseria gonorrhoeae is adept at avoiding both parts of the immune system: the innate and the adaptive immune system. The pathogen produces a variety of compounds that prevent innate immune recognition. Even when recognized, it can overcome innate immune attacks. For example, if eaten by immune cells called macrophages, it can survive inside them. It may even manipulate the macrophages from within and further suppress the immune response (reviewed here).
With respect to the adaptive immune system, Antibodies and T cells don’t effectively fight off repeat Neisseria gonorrhoeae infections. One reason is the pathogen frequently switches up its cell surface compounds. This renders any adaptive immunity obsolete as the bacteria multiply. Thus, Neisseria gonorrhoeae avoid continued detection and elimination (reviewed here and here).
Many Neisseria gonorrhoeae infections are asymptomatic. However, asymptomatic hosts can still spread the bacteria to others. Symptomatic infections cause a wide variety of painful and potentially devastating long-term complications. These include:
- painful urination
- pelvic inflammatory disease
- ectopic pregnancy
- eye infections (conjunctivitis) in newborns that can lead to blindness
Learn more about complications from Neisseria gonorrhoeae infection on the Mayo Clinic’s website.
Neisseria gonorrhoeae treatment
The frontline treatment for Neisseria gonorrhoeae infection is a course of antibiotics. However, as the CDC explains in this short video, Neisseria gonorrhoeae quickly evolves resistance to multiple antibiotics. Indeed, the antibiotic ceftriaxone is considered “our last treatment option” for this pathogen.
One reason Neisseria gonorrhoeae rapidly acquire resistance is they are particularly good at sharing DNA with one another. Thus, if one population of Neisseria gonorrhoeae evolves the ability to resist an antibiotic, others can quickly take up the DNA encoding that ability. As a testament to this adaptability, this pathogen makes use of all modes of antibiotic resistance:
- It uses so-called “efflux pumps” to pump antibiotics out of the cell
- It alters the structures of antibiotic targets to make them more difficult to bind
- It uses enzymes to breakdown the antibiotics
- It chemically modifies antibiotics to make them less effective
See Unemo et al 2019 for a more in-depth look at Neisseria gonorrhoeae antibiotic resistance.
The WHO recently conducted a study of countries tracking Neisseria gonorrhoeae antibiotic resistance. In 2015-2016, 23.8% of these countries already reported cases of Neisseria gonorrhoeae infection that are resistant or which have lower susceptibility to ceftriaxone. Multi-antibiotic treatments are possible, but new treatment options are still needed.
Preventing Neisseria gonorrhoeae infection
There are currently no effective vaccines for Neisseria gonorrhoeae. Yet, researchers are optimistic that vaccines are possible. Vaccines developed for similar bacteria recently showed some efficacy against Neisseria gonorrhoeae. In addition, the WHO recently renewed its focus on the development of a Neisseria gonorrhoeae vaccine. It convened a group of researchers to outline essential vaccine characteristics. The results of their discussions can be found here.
In the absence of vaccines, other important measures can be taken to curb the spread of gonorrhea.
- Sexual behaviors: Safer sex practices and regular STI testing can prevent Neisseria gonorrhoeae infection and transmission. Nonetheless, there were more than 85 million new cases of gonorrhea in 2016 (Rowley et al 2019). Infection is also on the rise (reviewed in Kirkcaldy et al 2019). Thus renewed efforts and new forms of treatment and prevention are essential.
- Early diagnosis: The WHO has called for the development of newer, less expensive diagnostics for Neisseria gonorrhoeae and other STIs. These will be particularly useful if they can detect antibiotic resistant infections. Such diagnostics could guide effective treatment. Inexpensive diagnostics could also make it easier to screen for asymptomatic infections. Asymptomatic screening could go a long way to decreasing the spread of this pathogen.
- Targeted prevention: Importantly, Neisseria gonorrhoeae infection is more prevalent in certain communities. These include sex workers and men that have sex with men (MSM) (Kirkcaldy et al 2019). Indeed, in one study of MSM in San Francisco, ~5% of those tested were infected with non-genital Neisseria gonorrhoeae (Johnson Jones et al 2019). This is much higher than the roughly 0.2% of all US men with reported Neisseria gonorrhoeae infection in 2019 (see CDC website). Tailoring prevention initiatives and messaging to these groups might effectively reduce Neisseria gonorrhoeae prevalence.
Outlook
There are disappointing trends in Neisseria gonorrhoeae infection and detection. Infections are on the rise. Additionally, STI screening decreased during the COVID-19 pandemic (Pinto et al 2021). Yet, there is reason to hope that we’ll be better equipped to fight this pathogen in the future. Some reasons for optimism include:
- Renewed focus on diagnostics. Since the start of the COVID-19 pandemic, there has been intense focus on diagnostics. There have also been many developments in this space (such as Mammoth’s own CRISPR diagnostics). Hopefully, we’ll be able to apply these diagnostics advancements to other diseases. Such advances may make it easier to screen for Neisseria gonorrhoeae infections globally.
- Increased focus on antimicrobial resistance. In the 2000s and 2010s there was a steady increase in research papers focused on antimicrobial resistance. There hasn’t been a similar increase in Google searches on the topic, but hopefully research will translate into public awareness. Pushing in this direction, the CDC is intensifying its focus on resistance through its Antibiotic Resistance Solutions Initiative.
- Actual and potential government action on antimicrobial resistance. The UK recently started an initiative that creates monetary incentives for creating new antimicrobials. In the US, a similar initiative (the Pasteur Act) is gaining traction. Hopefully, new antimicrobials are created in response to these initiatives. They may provide a lifeline in the fight against antimicrobial resistance.