Tyler Ford
01/21/2021
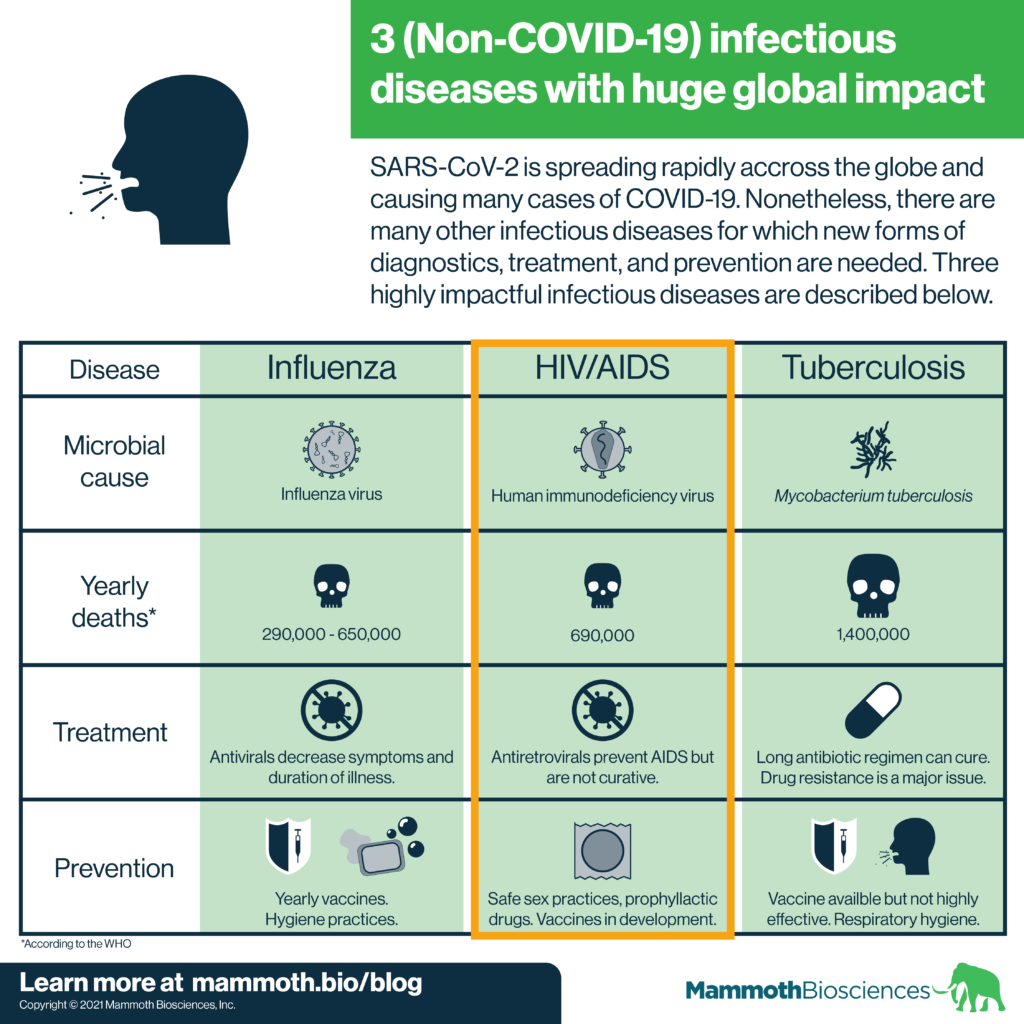
COVID-19 cases are soaring across the globe. The pandemic rightly takes up much of our attention. Yet, it’s important to remember that other infectious diseases continue to have huge global impacts. In this “Infectious Disease Spotlight” series, we cover 3 of the most globally impactful infectious diseases. Just as they are essential in our efforts to stop the spread of COVID-19, new diagnostics will help pave the way to controlling these diseases.
Check out our other posts on the flu, tuberculosis, Candida auris, Neisseria gonorrhoeae, Candida auris, and Clostridioides difficile.
Human immunodeficiency virus (HIV) infection results in about 690,000 global deaths each year according to the WHO. The virus spreads through contact between infected body fluids and mucosal tissue, blood, or broken skin (see review). Often, it is transmitted through sexual intercourse or needle sharing. HIV positive mothers can also transmit HIV to newborns during childbirth.
HIV itself isn’t the proximal cause of death in infected individuals. Instead, HIV infects specific kinds of immune cells called T cells. This causes flu-like symptoms within the first couple of months of infection. Then, these acute symptoms abate and the virus can remain dormant in the body for many years. Later, the virus remerges and kills off many T cells.
When T cell levels drop to a specific amount, HIV positive individuals are considered to have acquired immune deficiency syndrome (AIDS). Due to their drastic drop in immune cells, AIDS sufferers can succumb to minor infections and other complications. Even in the absence of a severe decrease in T cell counts, the appearance of one of these complications can also define AIDS. These complications, rather than the HIV virus itself, kill AIDS sufferers.
Researchers have been studying HIV since it was identified as the causative agent behind AIDS in the 1980s. We now know a lot about how this virus functions, but there’s no cure yet. However, we have discovered ways to prevent HIV infection from developing into AIDS. We can also largely prevent HIV positive individuals from transmitting the virus.
Preventing HIV transmission
First and foremost, we can prevent HIV transmission via behavioral changes. Safe sex practices (e.g. wearing a condom) prevent the disease from transmitting during sex. Needle exchange programs provide intravenous drug users with new needles. This prevents the widespread re-use and sharing of needles that can cause transmission.
Thankfully, intensive research has led to the development of many HIV/AIDS drugs. These drugs prevent HIV positive individuals from progressing to AIDS. They can inhibit just about every step of the HIV infection and replication processes. There’s a drug to stop everything from the binding of the virus to the cell surface to the replication of the virus’ genetic material to the release of virus from infected cells.
So-called antiretroviral cocktails are capable of suppressing AIDS progression indefinitely. The viral suppression wrought by these drugs also drastically reduces transmission. Indeed the use of antiretroviral cocktails can nearly eliminate transmission from mothers to newborns. These drugs also drastically improve quality of life for people who are HIV positive.
Researchers have also developed drugs that can prevent one from becoming infected with HIV. People take such drugs prophylactically. These drugs do not completely eliminate the risk of transmission. They should be used along with safe sex and other prevention behaviors. Nonetheless, they represent a huge step forward in preventing HIV infection.
HIV vaccines
There have been several attempts to create HIV vaccines. In 2009, one such vaccine showed partial effectiveness. However, this vaccine was not efficacious enough to stop the HIV/AIDS pandemic. Research efforts and clinical trials in this area are on-going.
Why no HIV cure?
HIV is very hard to cure because the virus inserts its genetic material into infected cells’ genomes. The virus can lie in wait in cells’ genomes for years. It is very hard to create drugs that specifically target these latently infected cells. It’s also difficult to trigger the immune system to specifically kill latently infected cells.
Nonetheless, there have been two cases in which blood stem cell transplants appear to have removed all traces of HIV from patients. In the first case from 2009, doctors transplanted blood stem cells from a donor with a deletion in a receptor protein known as CCR5. CCR5 is one of the receptors that HIV uses to enter cells. Doctors transplanted these cells into an HIV positive patient undergoing leukemia treatment. After transplantation, this patient appears to have been cured. In a second case reported in 2020, doctors conducted a similar transplant on an HIV positive patient. This patient appears to be cured as well.
While such cases are inspiring, they do not represent a practical cure. Blood stem cell transplants require doctors to deplete the patients’ original stem cells with chemotherapy. This is dangerous, expensive, and also compromises the patient’s immune system. As a result, stem cell transplants will not be feasible for most HIV infected individuals.
Scientists are actively working on ways to use CRISPR to eliminate HIV from patients’ genomes. Hopefully we’ll see progress in this area in the near future!
HIV/AIDS diagnostics
Like influenza, there are many diagnostics available for HIV. Current low cost tests are usually antigen and antibody based. These detect components of the HIV virus itself or patient antibodies that bind to the virus. These tests are not as sensitive as nucleic acid based tests. Many tests also have low sensitivity when testing for the virus in body fluids other than blood from a vein (see CDC HIV testing page for more info). Low cost nucleic acid-based diagnostics, like CRISPR diagnostics, could make it easier to diagnose HIV infection early. The development and widespread use of such tests could lower HIV transmission.
