Tyler Ford
12/01/2020
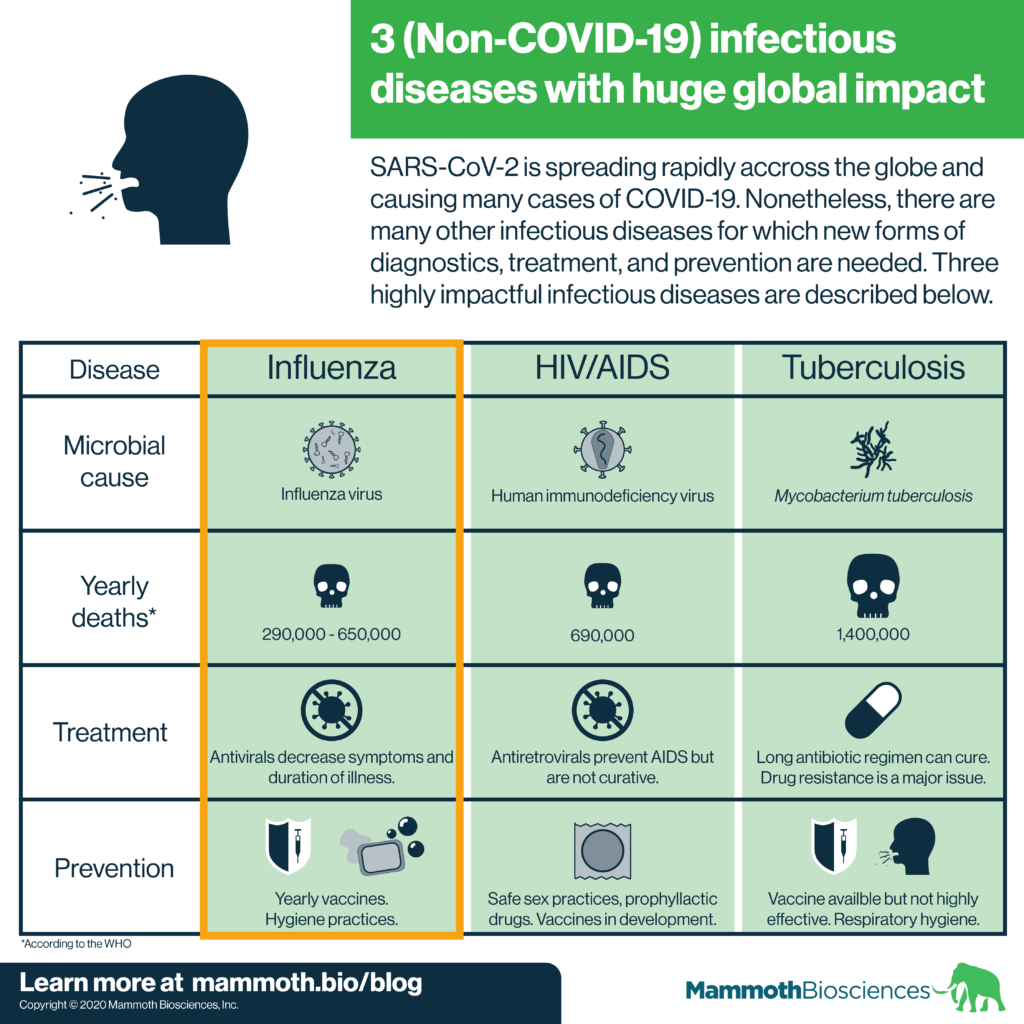
COVID-19 cases are soaring across the globe. The pandemic rightly takes up much of our attention. Yet, it’s important to remember that other infectious diseases continue to have huge global impacts. In this “Infectious Disease Spotlight” series, we cover 3 of the most globally impactful infectious diseases. Just as they are essential in our efforts to stop the spread of COVID-19, new diagnostics will help pave the way to controlling these diseases.
Check out our other posts on HIV/AIDS, tuberculosis, Candida auris, Neisseria gonorrhoeae, Candida auris, and Clostridioides difficile.
Learn about Mammoth’s CRISPR-based detection platform for SARS-CoV-2
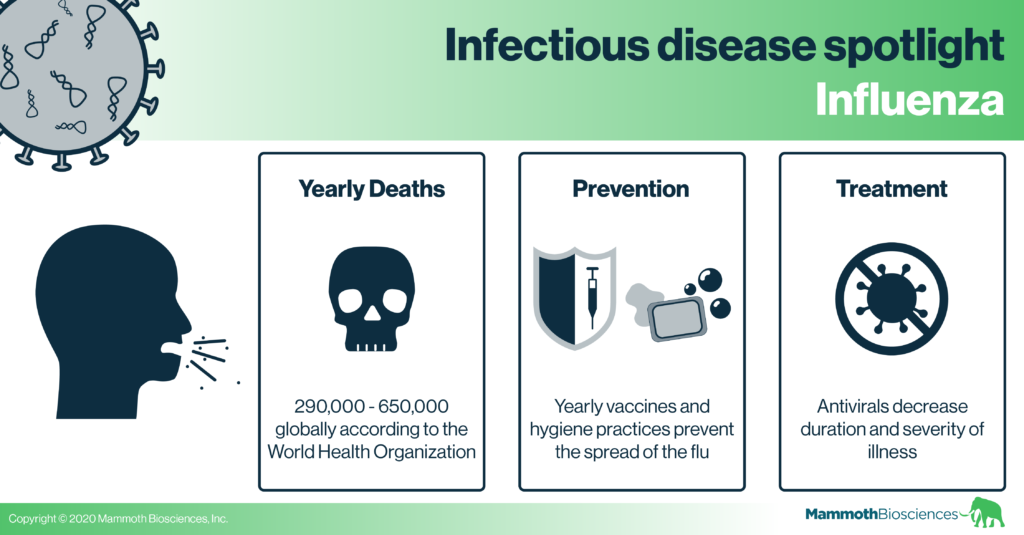
Influenza (the flu)
The flu virus infects columnar epithelial cells in the upper respiratory tract. In healthy individuals, some of these cells coat the respiratory tract in mucus. Others have hair-like projections called cilia. These beat foreign objects and pathogens out of the respiratory tract.
Stemming from the infection of these columnar epithelial cells, the flu has a wide range of symptoms. These include fatigue, cough, sore throat, congestion, sneezing, headache, and body aches (see CDC website for more info). These symptoms usually last less than two weeks. Yet, severe complications and even death can occur. In particular, individuals over the age of 65, under the age of 5, pregnant women, and those with chronic medical conditions are at high risk of complications from the flu.
Preventing flu transmission
We transmit the flu through small particle aerosols. Thus, we can prevent the spread of the flu using respiratory and general hygiene measures. These include covering coughs, using tissues, wearing masks, hand washing, and staying home when sick.
We can also prevent the spread of the flu with flu vaccines. Researchers create new flu vaccines each year. These target the flu strains predicted to be most prevalent that year. It is important to get a new vaccine each year because the flu evolves rapidly. You are unlikely to retain immunity to new strains year over year without a new vaccine.
Unfortunately, flu vaccines don’t always match circulating flu strains. This results in decreased immunity even if you do get vaccinated. Researchers are actively looking for ways to create pan-flu vaccines. These will protect against all flu strains.
Flu treatment options
Researchers have developed antiviral drugs for the flu. These decrease the severity and duration of flu infection. They disrupt the processes by which flu viruses empty their contents into cells. They can also disrupt the process by which new flu viruses leave infected cells. While these drugs can bring relief, they are not silver bullets. In addition, the flu can develop resistance to these drugs quickly. As a result, researchers are actively developing new drugs to treat the flu.
Flu diagnostics
There are many technologies available to diagnose the flu (see this Influenza review). Two of the most popular technologies for flu detection are antigen tests and RT-PCR. Antigen tests use antibodies to identify flu virus fragments in patient samples. They are the fastest and least expensive tests. Yet, antigen tests are less sensitive than RT-PCR which is considered the gold standard for specificity and sensitivity. RT-PCR detects segments of the flu genome. As we’ve discussed in other blog posts, RT-PCR is very useful but requires complex lab equipment and expertise to run. It is also expensive.
Thus neither rapid antigen tests nor RT-PCR are perfect. Other reasons we need new diagnostics for the flu include:
- The flu is often diagnosed based on symptoms. This can lead to incorrect diagnosis and treatment regimens. E.g. healthcare providers may mistakenly prescribe antibiotics for the flu (see estimates for inappropriate antibiotic prescriptions in the US here).
- We need less expensive flu diagnostics. These could be made available to people in low-income regions and better direct effective treatments in these regions.
- Rapid, nucleic-acid based diagnostics may make it easier to identify drug-resistant flu strains. Knowing that a flu strain is resistant to a drug is useful. Such knowledge can prevent healthcare providers from using ineffective antiviral compounds for treatment.
We’ve seen rapid advances in diagnostics in response to the COVID-19 pandemic. Hopefully advances in this field will be transferable to other infectious diseases. CRISPR diagnostics, in particular, can be rapidly adapted to detect the flu. CRISPR diagnostics should have the specificity and accuracy of RT-PCR and the rapidity/affordability of antigen tests. The pandemic is devastating, but it may have made an opening for advances in our fight against diseases as commonplace, but impactful as the flu.
In our next “Infectious disease spotlight” we’ll cover HIV/AIDS.
