Tyler Ford
07/28/2020
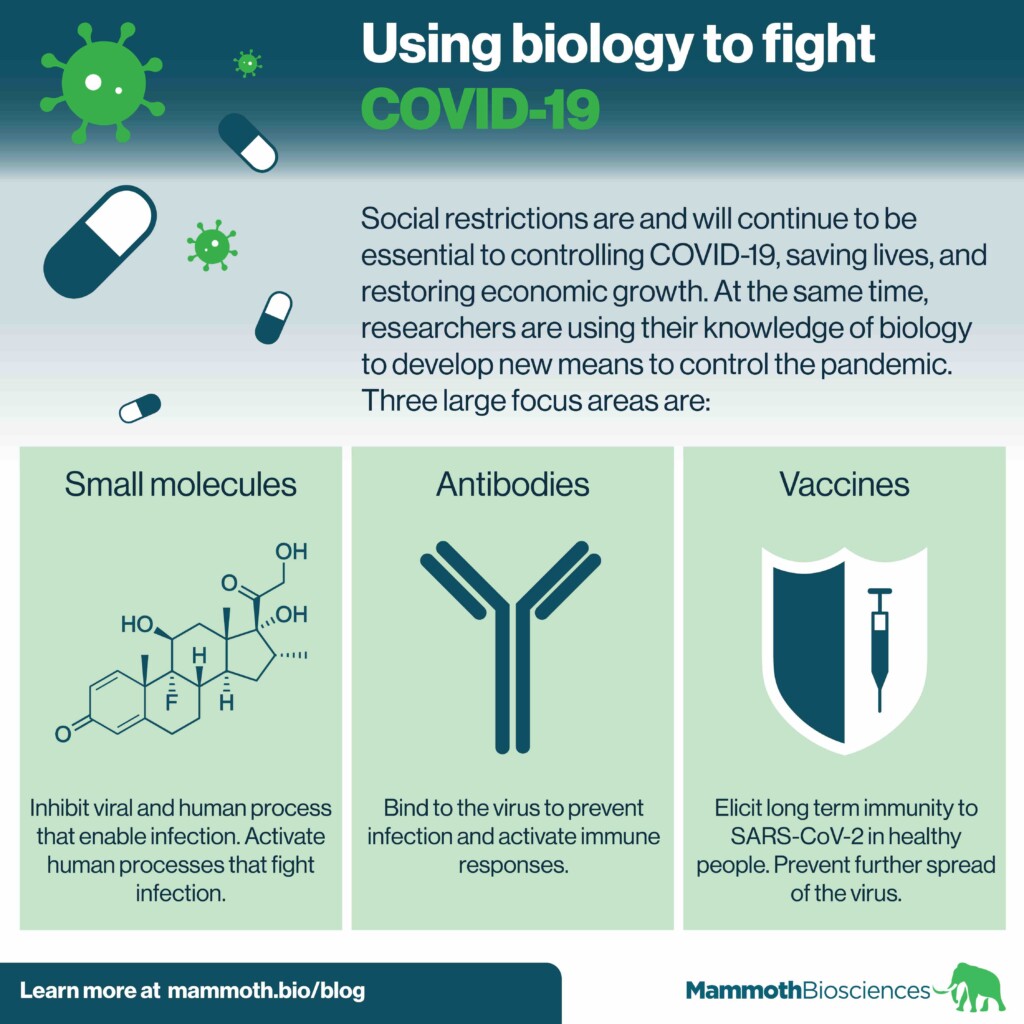
The COVID-19 pandemic is one of the greatest public health challenges we’ve faced in the last century. Social restrictions are and will continue to be essential to controlling the disease, saving lives, and restoring economic growth. Researchers and healthcare workers are also using their knowledge of biology to develop new means to control the pandemic. Three large focus areas are:
- Small molecules
- Antibodies
- Vaccines
Small molecules and antibodies are already helping healthcare workers treat COVID-19 patients. Vaccines will help control the pandemic in the long term. In this post, we provide a quick primer on these three areas of research.
What are small molecules, antibodies, and vaccines?
Small molecules
Small molecules are chemical compounds small enough to enter cells. These compounds usually slow or prevent infection in one of two ways:
- By interacting with the virus itself. Usually these small molecules inhibit a viral process.
- By interacting with the human body. Such small molecules may inhibit a body process that the virus needs to survive. Alternatively, they may activate body processes that fight the virus.
An example of the first kind of small molecule is Remdesivir from Gilead Sciences. SARS-CoV-2 is the virus that causes COVID-19. Remdesivir inhibits an enzyme that SARS-CoV-2 uses to copy its RNA genome. Thus, Remdesivir makes it difficult for the virus to copy itself. Remdesivir can decrease the length of hospital stays for COVID-19 patients. Yet, it is not a silver bullet. It helps patients but is not a dramatic cure.
An example of the second type of small molecule is a steroid called Dexamethasone. Some of COVID-19’s most devastating effects are thought to be due to over-activation of the immune system. Dexamethasone dampens the immune system. Clinical trial results show that dexamethasone decreases deaths of patients on ventilators or oxygen.
Scientists are searching for other small molecules to treat COVID-19. For example, researchers recently used a CRISPR screen to identify genes important for SARS-CoV-2 infection. Some of the proteins encoded by these genes enable infection. Others inhibit infection. The researchers additionally identified small molecules that inhibit some of these proteins. This and similar studies may accelerate the development of COVID-19 treatments.
Antibodies
The immune system creates antibodies in response to disease-causing agents (pathogens). Antibodies bind to pathogens. In doing so, antibodies can block pathogens from interacting with the body. Antibodies can also recruit other parts of the immune system to fight pathogens.
Researchers are learning to use antibodies to treat COVID-19. One way they’ve been doing this is by testing convalescent sera. This is essentially an antibody-containing portion of blood from patients who have recovered from COVID-19. Researchers have been using convalescent sera to treat newly infected patients with some signs of success.
Often, therapeutic antibodies bind to the SARS-CoV-2 spike protein. This protein gives the virus it’s crown-like appearance. It is the reason for the name “coronavirus”. The spike protein also enables the virus to enter cells.
Researchers are learning what interactions between antibodies and the spike protein lead to the best defenses against SARS-CoV-2. With this knowledge, companies are actively working to streamline the production of antibodies to treat COVID-19.
Researchers have additionally identified antibodies that bind to different parts of the spike protein. These individual antibodies effectively prevent infection. They can also prevent infection in combination. Using such combinations of antibodies may be important for future treatments. This is because viruses like SARS-CoV-2 acquire mutations when they multiply in patients. These mutations can prevent antibodies from binding to the virus. Yet, it is unlikely that the virus will acquire mutations that prevent antibodies from binding to separate sites. Thus, antibody combinations may lead to more effective treatments.
Although promising, antibody therapeutics can be more difficult to administer than small molecules. They are large and generally can’t be taken in pill form. They don’t easily travel across the gut and into the bloodstream. Instead, antibody drugs are usually delivered either by injection or IV infusion.
Even with the challenges of delivery, antibodies can be very effective. Indeed antibodies against Ebola can greatly decrease the mortality of this devastating disease. The FDA recently issued an emergency use authorization for a monoclonal antibody treatment for COVID-19 from Eli Lilly as well as for a similar treatment from Regeneron.
Vaccines
Vaccines are one of the main long-term hopes for stopping the pandemic. Vaccines come in many different forms but they all have the same goal. They make the body develop immunity to SARS-CoV-2 without causing major disease.
Generally, vaccines consist of small parts of a virus, broken parts of a virus, or dead whole viruses. In vaccination, healthcare workers introduce these to the body in a controlled way. Doing so, they can trigger the immune system. It will create antibodies and other immune responses. These can fend off later infection by the whole, live virus.
The best vaccines trigger long-lasting immunity that prevents people from getting sick. They also prevent viruses from spreading. Unfortunately, it is not 100% clear how to elicit immune responses that do these things. Thankfully, many researchers are developing COVID-19 vaccines. Some of these have elicited promising immune responses in animal models.
Indeed, there have been some early positive results from the clinical trials for COVID-19 vaccines. Pfizer recently published a press release indicating that their vaccine is 90% effective at preventing symptomatic COVID-19. Moderna similarly published a press release indicating that their vaccine is 95% effective. AstraZeneca announced that it’s vaccine has varying levels of efficacy depending on the dosing regimen with its average efficacy at 70%.
Future protection from COVID-19
While highly effective vaccines are a long-term means of fighting the pandemic, they require large-scale production, distribution, and public acceptance. In addition, there is no guarantee that a SARS-CoV-2 vaccine will protect us from all future forms of the virus. Like the flu, yearly vaccinations may be necessary to prevent COVID-19 resurgence.
Thus, it’s essential to continue developing a variety of means of fighting COVID-19. We must also continue to develop diagnostics that enable us to identify infection and implement effective public health policies. Only then can we control the most devastating effects of the pandemic.
Read our white paper – A protocol for rapid detection of SARS-CoV-2 using CRISPR: SARS-CoV-2 DETECTR
Learn about our CRISPR-based SARS-CoV-2 detection platform for commercial labs!
