Tyler Ford
08/18/2020
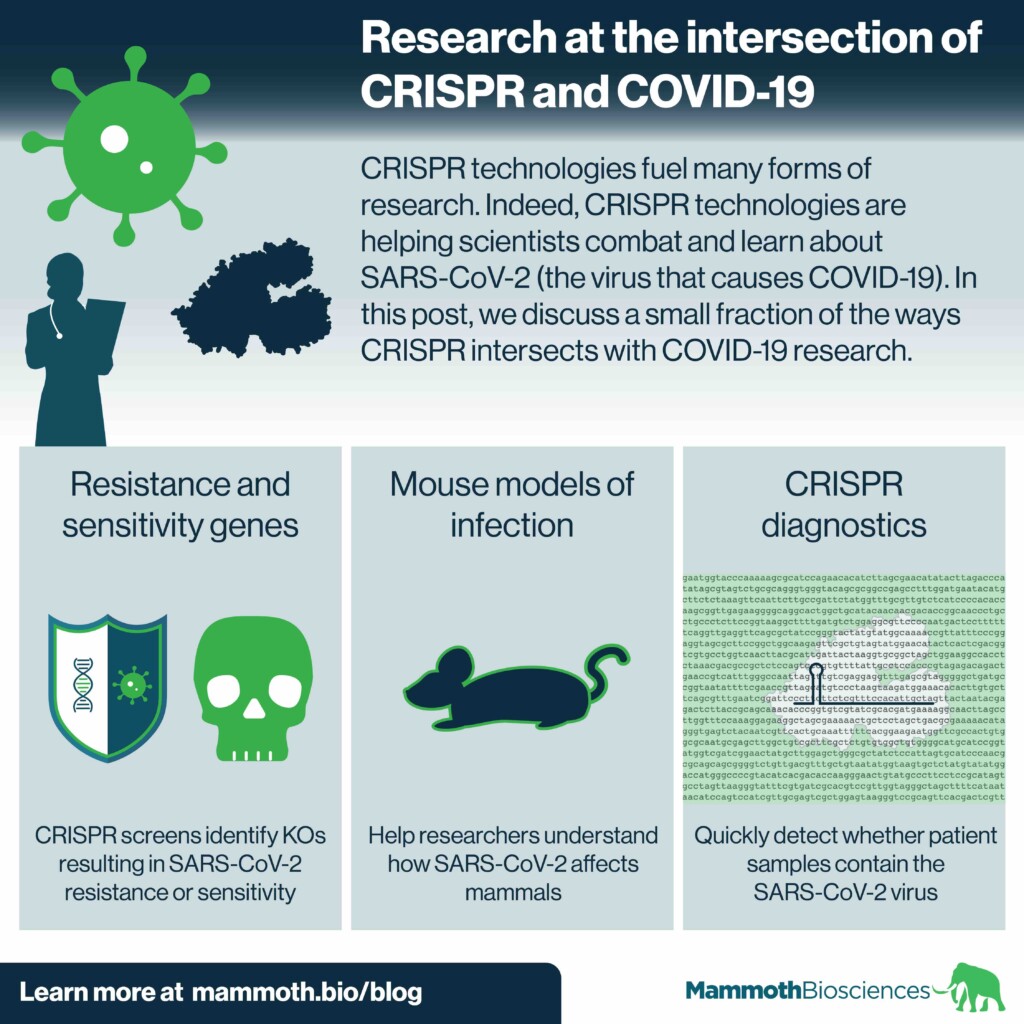
CRISPR technologies fuel many forms of research. Now, they’re helping scientists combat and learn about SARS-CoV-2 (the virus that causes COVID-19). In this post, we discuss a small fraction of the ways CRISPR intersects with COVID-19 research.
Learn how researchers expand the CRISPR toolkit
Using a CRISPR screen to identify SARS-CoV-2 resistance and sensitization genes
In a recent bioRxiv preprint, Wei et al performed a genome wide CRISPR screen to identify genes that either increase or decrease cell viability upon SARS-CoV-2 infection. The researchers performed the screen using a kidney cell line from Chlorocebus sabaeus monkeys. This cell line is highly susceptible to SARS-CoV-2 infection.
The knock-outs (KOs) that led to increased viability (KO leads to “resistance”) targeted some expected and unexpected genes. Among the expected were ACE2 and CTSL. ACE2 encodes the receptor SARS-CoV-2 uses to enter cells. CTSL encodes a protease involved in priming SARS-CoV-2 for cell entry. Among the unexpected were genes involved in chromatin remodeling and cell signaling.
In the knock-outs that led to decreased viability (KO leads to “sensitization”), the authors identified histone chaperone proteins as particularly strong hits.
After validating many of their hits in additional KO experiments, the researchers checked if they could target some of their hits with known inhibitors. Indeed, they found that inhibiting a few of the proteins whose KO led to resistance resulted in increased viability after infection with SARS-CoV-2.
The authors hope that their work can lead to the development of host-directed therapies.
Along similar lines, Bailey and Diamond 2020 summarized the work of multiple researchers who used CRISPR screens to identify genes impacting the SARS-CoV-2 lifecycle. The hits included many different kinds of genes involved in such processes as attachment to the host cell, entry into the cytoplasm, and exit from the host cell. It’s possible that future efforts to target these genes and their encoded proteins could lead to new treatments for coronavirus infection.
Mouse model for SARS-CoV-2 infection
Researchers use mice to get a basic understanding of how diseases impact mammals like us. However, SARS-CoV-2 does not infect mice. Part of the reason for this is mice have a different version of the receptor, ACE2, that the virus uses to get into cells.
In a recent Cell Host and Microbe paper, Sun et al used CRISPR genome editing to replace mouse ACE2 with human ACE2. SARS-CoV-2 successfully infects the resulting “humanized” mice. Indeed, the infected mice recapitulate some of the characteristics of infection in humans. E.g., the virus infects many of the same tissues in mice and older mice have more severe symptoms than younger mice.
Mice expressing the human ACE2 receptor have been created in the past. Yet, these were created using transgenic technologies. Such technologies inserted the receptor at random locations in the mouse genome.
More precisely genome edited mice may better recapitulate the etiology of human COVID-19. These mice will hopefully be useful for understanding how COVID-19 impacts the body. They may also help researchers weed out ineffective treatments.
CRISPRDx for COVID-19
We described an early version of our CRISPR-based SARS-CoV-2 DETECTR™ in Nature Biotechnology. This CRISPR diagnostic (CRISPRDx) makes use of Cas12. When directed to the SARS-CoV-2 RNA genome, Cas12 first cleaves the genome. Then it cleaves reporter molecules. This results in visible signals (fluorescence or lines on a test strip), and the CRISPR chemistry is compatible with deployment in both centralized laboratories and decentralized product formats, such as a disposable Point-of-Need device. This early version of our SARS-CoV-2 detector effectively identifies SARS-CoV-2 in patient samples. It has 95% positive predictive agreement and 100% negative predictive agreement with a qPCR assay from the CDC.
Learn about our CRISPR-based SARS-CoV-2 detection platform for commercial labs!
