Tyler Ford
04/07/2022
All of our organs are marvels of evolution, and the liver is no exception. The liver intimately interacts with the bloodstream and is the first stop on the blood’s journey from the gut to the rest of the body. The liver carries out numerous activities to determine whether our metabolic needs are met and distribute nutrients to other organs. It also provides protective functions both detoxifying harmful compounds and defending us against a variety of pathogens. All the while, the liver sends and responds to signals determining whether nutrients like glucose need to be stored or released and creates bile acids that help us digest a variety of foods (Shulze et al 2019).
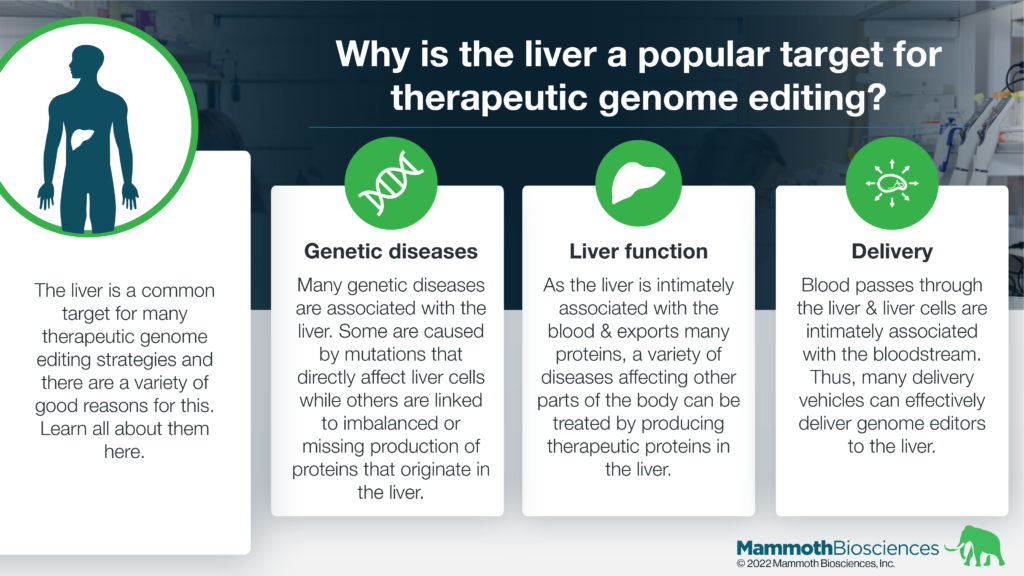
Recently, liver cells have emerged as important targets for therapeutic genome editing. The reasons why stem from the liver’s status as a vital, multi-functional organ. Below we’ll cover three of these reasons in-depth:
- There are many rare genetic diseases that are associated with or may be impacted by protein production in the liver
- Proteins produced in the liver can impact many other organs and systems due to the liver’s intimate association with the blood
- Researchers have various means of targeting particular types of liver cells with genome editing technologies
Treating rare genetic diseases through liver genome editing
There are a variety of rare diseases that are associated with the liver. Many of these diseases are caused by mutations in genes encoding proteins that carry out important functions in liver cells. Others aren’t necessarily caused by mutations that affect liver cells directly but can be treated by producing therapeutic proteins in the liver. Collectively these diseases cause illness and suffering for millions of people all over the world.
Given the liver’s diverse array of functions, it is perhaps unsurprising that small changes to liver genes and cells can lead to or treat disease. Indeed, this provides clinicians and researchers with a great opportunity. If they can effectively get genome editors into the right liver cells, they can potentially treat/cure a large number of ailments. They can even treat diseases that primarily impact other parts of the body because many proteins produced in the liver can be transported to other tissues through the blood.
Some of the many diseases associated with the liver include:
- Alagille Syndrome
- Wilson disease
- Hemochromatosis
- Non-alcoholic fatty liver disease
- Alpha-1 antitrypsin deficiency
- Biliary atresia
- Lysosomal acid lipase deficiency
- Hepatic porphyria
- Autoimmune hepatitis
- Primary biliary cholangitis
- Primary sclerosing cholangitis
- Hemophilia
And you can learn more about many diseases of the liver on the American Liver Foundation website.
That’s not to say that developing cures for these various diseases will be “easy.” After all, researchers need a good understanding of these diseases as a starting point and we still have much to learn about many of them. In addition, even when we understand a disease well, researchers need ways to avoid editing the wrong DNA sequences, to prevent editing in the wrong cells, and to ensure that any proteins produced as a result of editing are created in the right, therapeutic doses for the right duration. Nonetheless, liver genome editing offers a clear avenue to treat a wide variety of rare diseases.
As you’ll learn in the next section, some of the potential problems associated with therapeutic genome editing are inherently easier to surmount when working with the liver as compared to other organs.
Delivery to the liver
One of the most common issues with in vivo genome editing is the lack of effective ways to deliver genome editors to the right cells. However, some popular delivery vehicles including adeno-associated viruses (AAVs) and some lipid nanoparticles (LNPs), effectively transport their cargoes to the liver (Colella 2018, Finn et al 2018). This “tropism” for the liver is partially due to the fact that the liver is so intimately associated with the blood. Indeed, one of the liver’s key functions is to detoxify foreign compounds and uptake lipids like those found in LNPs.
Importantly, researchers don’t generally want to deliver genome editors to just any liver cells. They usually target hepatocytes – the non-structural liver cells that carry out many of the liver’s functions. There are other types of liver cells, and if genome editing payloads are directed towards these cells, it can decrease the effectiveness of therapeutic genome editing. Thankfully, years of research in gene therapies have given scientists a variety of means to prevent delivery to these other liver cells (Jacobs et al 2012). Researchers are also developing new ways to achieve more specific delivery to hepatocytes. These include efforts to alter the protein and lipid compositions of AAVs and LNPs, respectively, for more favorable cell targeting (Colella 2018, Witzigmann et al 2020).
Finally, researchers have a lot of experience targeting the liver. Thus, they know how to handle many issues and side effects that can manifest with liver-targeted therapies. This know-how enhances the potential for success with such therapies.
Genome editing beyond the liver
Of course, the liver is not the only organ researchers wish to target through in vivo genome editing. Many other organs could be targeted to treat other diseases (neurological diseases via the brain for instance). Yet, liver genome editing is a great potential proof point thanks to its association with a wide variety of diseases, diverse natural functions, and delivery possibilities. Many patient lives have the potential to be saved or improved through liver genome editing and researchers will be able to apply many of the things they learn from targeting the liver to other organs.