Tyler Ford
09/01/2020
COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, can have health impacts ranging from mild to deadly. Researchers are in the process of learning how and why some people get severe disease while others are asymptomatic. There is still a lot to learn, but, in this post, we cover the basics of how SARS-CoV-2 impacts the body.
Early and mild disease
SARS-CoV-2 is primarily transferred via respiratory fluids including droplets and aerosols. When the virus enters the body, it first infects cells in the upper respiratory passages that lead to the lungs. It does this by attaching its spike protein to a cellular receptor called ACE2. Once attached via the spike, the virus fuses its membrane with that of the infected cell (see Shang et al 2020). The infected cell then takes up the virus’s genetic material and uses the information encoded within to create more viruses. Later, these viruses burst out of the cell.
In asymptomatic and mild cases, the infection may spread no further than the upper respiratory passages. In these cases, it’s possible that the immune system will easily controls the infection. Why is unclear. Among the possibilities: there may be less virus to start off with or these patients may have some preexisting immunity. Such pre-existing immunity may be due to previous infection by similar coronaviruses. Vaccinated individuals can also quickly eliminate the virus before it causes any damage.
Moderate to severe infection
In more severe cases, SARS-CoV-2 infection can spread deep into the lungs. In particular the virus can get into the cells that are at the border of the lungs and the blood stream. Here in the “alveoli”, oxygen and CO2 are exchanged with the blood.
In addition to effects caused by direct infection, infected cells recruit the immune system. In the process of eradicating the virus, the immune system kills more infected cells. This further disrupts the lungs. Sometimes this can cause massive damage to the barrier between the blood vessels and the lungs. As a result, liquid can enter the lungs causing further breathing and oxygen transfer issues.
When the virus kills the cells lining the lungs, it can gain access to the blood and spread to other organs. Because ACE2 is expressed in many tissues, SARS-CoV-2 can effectively infect and kill cells in many organs.
How SARS-CoV-2 impacts other organs is an area of intense investigation. If you’d like to learn more about its effects in other organs, see this STAT article.
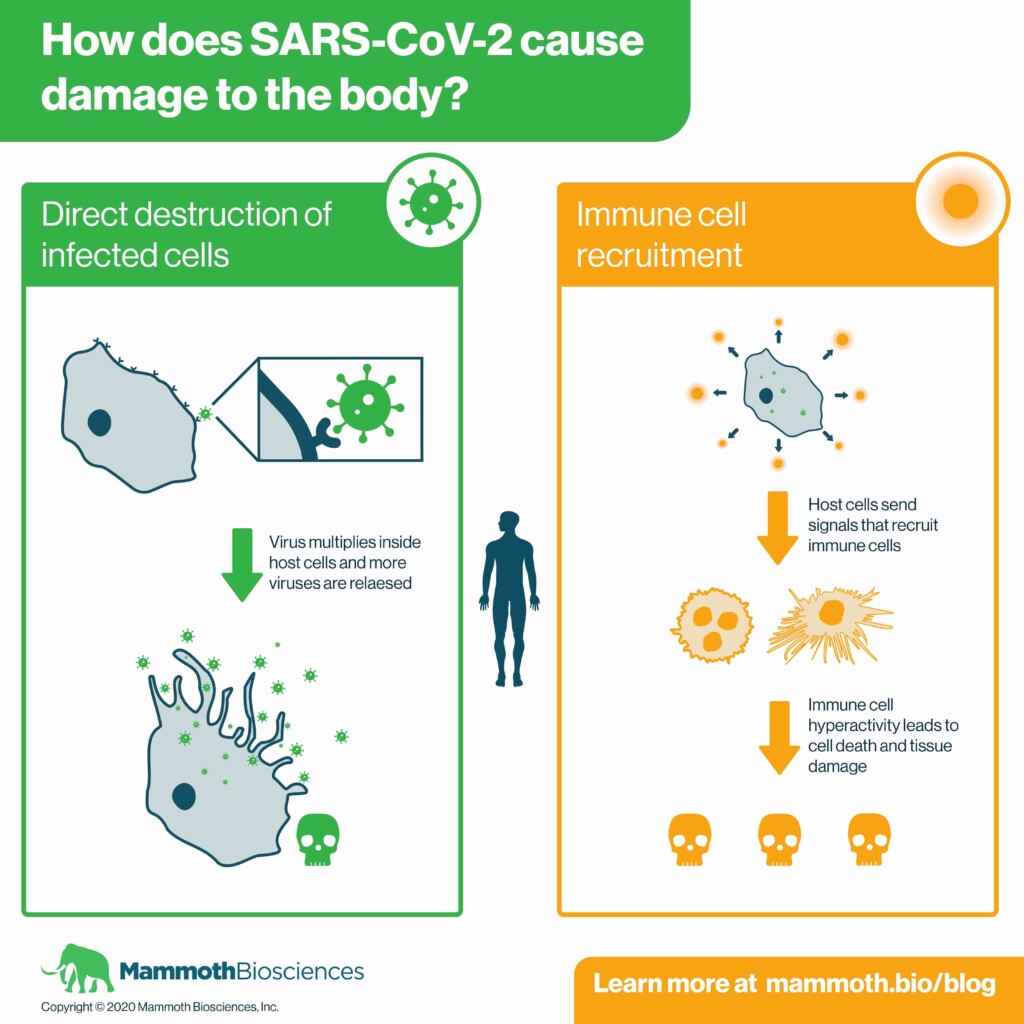
Overall, the same two processes are at work in the lungs and other organs:
- The SARS-CoV-2 virus causes direct damage by killing cells.
- The immune system causes additional damage by killing infected cells and causing collateral damage to nearby cells.
For many severe cases of COVD-19, the immune system can eventually overcome the virus — usually with the aid of physicians who slow the spread of the virus and tamp down the immune system. However, the damage wrought by SARS-CoV-2 and the immune system can have lingering effects for COVID-19 patients. Even those with “mild” cases can become so-called “long haulers” who have symptoms that linger for months.
In our post titled, “Small molecules, antibodies, and vaccines: Using biology to fight COVID-19” you can learn more about the drugs researchers and physicians are developing to prevent SARS-CoV-2 infections and tamp down the immune system.
The age connection
As you may have heard, younger individuals are often but certainly not always, spared from the more devastating effects of SARS-CoV-2 infection. Nonetheless, studies have shown that younger and asymptomatic individuals can harbor large amounts of virus. Given their high levels of virus, it is reasonable to expect that children and asymptomatic people can still spread the virus to others.
To prevent the spread of the virus, eligible individuals should, first and foremost, get vaccinated. It’s also essential that we adhere to public health measures such as wearing masks and social distancing. In addition, increasing overall testing capacity will make it easier for individuals to determine if they’ve been infected. In particular, inexpensive and rapid diagnostics will enable us to decentralize testing. If we can detect infected individuals early, we can prevent them from infecting those who are more susceptible to severe disease.
Check out this post to learn how “Point-of-Need” diagnostics will make it easier to rapidly test and isolate asymptomatic individuals.
Learn about our CRISPR-based SARS-CoV-2 detection platform for commercial labs!
